Finger Nail Fungus vs. Other Nail Issues: How to Tell the Difference
Getting to Know Finger Nail Fungus and Other Nail Troubles
When it comes to keeping our nails in tip-top shape, it helps to know the ins and outs of different nail conditions. Take finger nail fungus, for example – it’s more common than you might think, yet people often mix it up with other nail issues. In this read, we’re chatting about what finger nail fungus really is, how it differs from other nail problems, and why keeping your eye on these details is so important. We’ll dive into what to watch out for, talk about the symptoms, and shed some light on effective treatments. So whether you’ve noticed just a hint of change in your nail’s appearance or you’re dealing with a stubborn problem, being clued in is the first step to achieving those healthy nails you love.
It’s worth noting that finger nail fungus isn’t merely a cosmetic nuisance—it’s your nail waving a red flag about an infection that needs some care. And while other nail issues like psoriasis, damage from injuries, or even bacterial infections can look pretty similar, knowing which one you’re facing is key because the treatments are worlds apart. With the right mix of awareness and care, you can stop minor problems from snowballing into something more serious. Let’s take a closer look at what really sets finger nail fungus apart from other nail nuisances in our quest for better nail health.
So, What Exactly is Finger Nail Fungus?
Finger nail fungus is essentially an infection that creeps into your nail bed courtesy of various fungal organisms. You might notice it as a discoloration of your nail—perhaps a yellowish hue, thickening, or even areas where the nail seems to crumble. While many people shrug it off as just a cosmetic blemish, this pesky infection can create bigger problems if it’s not treated in time. It loves warm, damp places (think sweaty gym locker rooms or communal showers), which makes your fingers especially vulnerable after contact with less-than-clean surfaces. Understanding how it works is the first step to spotting it and tackling it head-on.
Often, the infection starts off slow—maybe with a few tiny white or yellow spots that gradually spread. In more pronounced cases, the nail might get brittle or warped, leading to discomfort or even interference with your day-to-day activities. What makes this fungal fellow so tricky is how easily it can masquerade as another nail condition, leading to confusion and misdiagnosis. So, keeping an eye out for subtle cues like an odd texture or unexpected color changes can really help you catch it early.
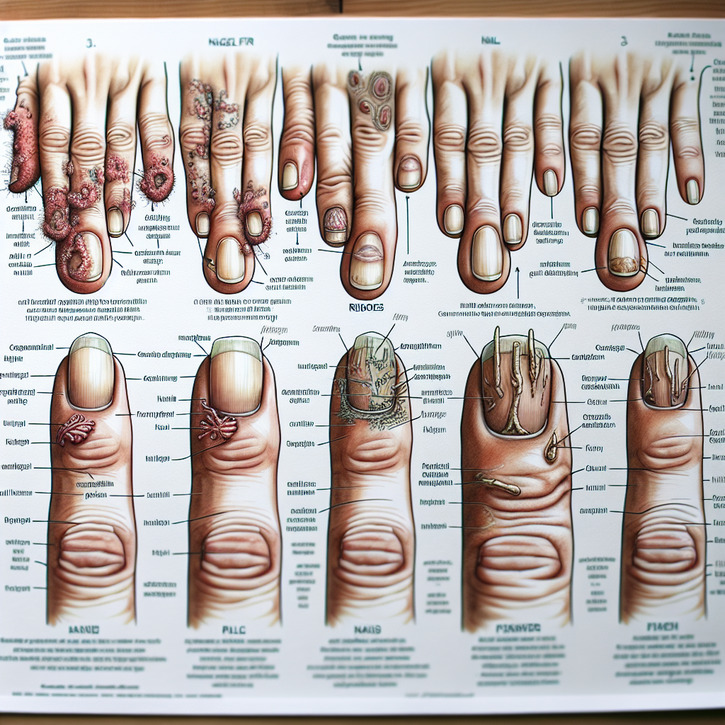
A Quick Look at Other Nail Disorders
Nails can face all kinds of issues beyond fungal infections. For example, psoriasis can cause pits, ridges, or even result in the nail peeling away from the nail bed. An injury might leave you with bruising or a permanently altered nail shape, and bacterial infections could lead to swelling and pain around the nail. With such a diverse lineup of nail troubles, pinpointing exactly what’s going wrong is essential for choosing the right treatment. By comparing finger nail fungus with these other conditions, you’ll see there are definitely some standout differences in how they show up and progress.
Sure, many nail issues share common traits like discoloration or thickening, but their underlying causes and needed treatments can be vastly different. Getting it right means avoiding unnecessary or even counterproductive remedies, and making sure you get a solution that's tailored to the problem at hand. Whether your nail problem stems from an infection, your body’s immune response, or physical trauma, each scenario has its quirks that really call for a specialized approach.
Why It’s So Important to Tell Nail Issues Apart
Sorting out different nail problems isn’t just about nailing the right diagnosis—it’s a critical part of effective treatment too. Mistaking finger nail fungus for something like psoriasis or a bacterial infection might lead to the wrong approach, prolonging discomfort unnecessarily. When you’re spot-on in identifying the culprit, you and your healthcare provider can craft a strategy that directly targets the problem. Plus, choosing a tailored treatment plan can lower your chances of the issue coming back or getting worse.
Being proactive with clear identification also means you know what habits to steer clear of and how to adjust your nail care routine. Whether it’s about choosing the right antifungal medications, keeping up with smart hygiene practices, or even tweaking your lifestyle a bit, knowing exactly what’s causing the nail trouble sets you on the path to better nail health. In simpler terms, getting to the bottom of the issue makes all the difference when it comes to prevention and effective treatment.
Catching the Early Signs of Finger Nail Fungus
Spotting finger nail fungus early on can really make life easier, as you can kick in treatment before things get too out of hand. You might first notice a subtle change in color—perhaps your nail turns a bit yellow, white, or even brown around the edges. The nail might also take on a thicker or crumbly texture, sometimes even lifting away from the nail bed. These visual hints may seem trivial at first, but they could be your cue that fungus is at work. Paying close attention can save you a lot of hassle down the line.
Along with these visual clues, you might experience slight discomfort, a mild ache at the base, or maybe even a faint odor. These early signals might feel like nothing more than everyday wear and tear, but they actually serve as early warnings to nip the issue in the bud. Compared to other nail conditions, the fungal infection tends to develop gradually, often following environmental exposures, which makes its pattern a tad unique.
To put it into perspective, conditions like nail psoriasis often show up as pitting or the nail peeling away from the skin, while bacterial infections are more prone to causing sudden swelling and redness. Although the symptoms can overlap, carefully noting the small differences can help you figure out what’s really going on. For instance, finger nail fungus rarely causes immediate pain, unlike injuries from physical trauma—so keeping an observant eye is really key.
What Your Eyes Can Tell You: Visual Signs
One of the biggest giveaways for finger nail fungus is the nail’s overall makeover. You might see discoloration—think white spots, a yellowish tint—or notice that the nail thickens, creating a bumpy appearance. In serious cases, the nail might even crumbly or separate from the nail bed. These visual changes are often what drive people to consult a professional, as they signal that there’s more going on beneath the surface.
Changes usually occur slowly enough to let you catch even the smallest alterations—like a slight color change at the nail’s edge or a bit of thickening here and there. Even if you chalk it up to aging or minor wear, a persistent change is a strong hint of an underlying fungal infection. Keeping tabs on your nail’s health, especially if you’re often around moisture or shared surfaces, is a smart move to ensure early treatment.
Early Warning Signs You Shouldn’t Ignore
Early symptoms of finger nail fungus can be pretty subtle—so subtle that it’s easy to miss them amidst everyday life. At first, you might not feel any discomfort, which is why these early signals can slip under the radar. However, besides those minor visual cues, you might pick up on a slight odor or a little extra thickening of the nail over a few weeks. Recognizing these early signs is key because getting in early usually means a smoother, quicker treatment.
Too often, people dismiss these initial changes as just a bit of normal wear and tear, only to find out later that the condition has worsened. It’s precisely these sneaky early indicators that let you know a fungal intruder might be at work. With proper attention, you can differentiate finger nail fungus from other nail issues and take prompt steps, like visiting a professional, to get it under control. The catch is to stay alert to any changes, no matter how minor they might seem.
How Finger Nail Fungus Stacks Up Against Other Nail Problems
When you compare finger nail fungus with other nail issues, it’s a bit like comparing apples and oranges. Unlike nail psoriasis, which might show tiny pits or separation of the nail from its bed, fungal infections tend to have a more even spread of discoloration and thickening that starts right at the edges. And while bacterial infections can cause rapid swelling and redness, fungus makes its move in a much more gradual fashion. Its unique blend of odor and texture really sets it apart.
Then there are nail problems resulting from trauma, where a clear history of injury usually points to the issue. In contrast, finger nail fungus creeps along slowly, sometimes lying low before you even notice anything amiss. It’s these subtle differences that can help you pinpoint whether your nail changes are caused by an infection or another underlying issue. While many signs might overlap, the nuances in progression are often the puzzle pieces you need for a proper diagnosis.
What’s Behind the Infection? Causes and Risk Factors
Finger nail fungus tends to thrive in warm, damp environments—making places like public showers and gyms the perfect hangouts for these fungi. The infection typically kicks off when a nail comes into contact with contaminated surfaces, especially if there’s already a tiny break in the nail or nearby skin. On the flip side, other nail issues like psoriasis or trauma arise from very different causes: genetic factors, autoimmune responses, sudden blows, or repetitive stress.
Lifestyle choices also play a starring role when it comes to developing finger nail fungus. Frequent visits to nail salons that might not follow rigorous sterilization practices, extended exposure to water, or neglecting proper hygiene can all set the stage for an infection. In contrast, other conditions might be tied more to your genetics or external injuries rather than an infectious agent. So, understanding these varied risk factors can really help you tailor a prevention and treatment plan that fits your situation.
It’s also interesting to note that environmental factors can add fuel to the fire. People living in warmer, more humid climates are generally at higher risk compared to those in drier areas. This just underscores why it’s so important to keep your hands and nails dry and clean, especially after you’ve been in moist surroundings. Unlike other nail problems that might not share these specific risk factors, fungi definitely love the damp life.
Unmasking the Culprits Behind Finger Nail Fungus
The main villains behind finger nail fungus are dermatophytes, yeast, and even non-dermatophyte molds that manage to breach the nail’s natural defenses. These organisms often seize the opportunity when the nail’s barrier is compromised—be it from minor injuries, extended moisture exposure, or other factors. Unlike autoimmune issues or physically traumatic damages, the root cause here is straightforward: a fungal infection that calls for targeted antifungal treatment.
Getting a handle on which specific fungus is causing the trouble allows healthcare providers to pick the most effective antifungal agent. This methodical, evidence-based approach helps avoid the pitfalls of mistakenly treating a non-infectious condition with overly aggressive measures. Knowing that the underlying culprit is an infectious agent sets finger nail fungus apart from other nail disorders that might look similar at first glance.
How Lifestyle and Environment Factor In
For many folks, continuous exposure to damp conditions—like frequent washing or working in humid environments—plays a big role in inviting finger nail fungus to take hold. Not only does a moist environment serve as a nurturing bed for these fungi, but shared spaces like locker rooms or swimming pools can also be hotspots for these unwelcome visitors. On top of that, neglecting to dry your nails properly can give fungi the perfect chance to flourish. This is quite different from nail issues caused by injuries or genetic factors, where moisture isn’t the main culprit.
Even choices like wearing tight, non-breathable gloves for long stretches can backfire, creating a snug, humid setting that fungi really love. Understanding these nuances in lifestyle and environmental risks can lead you to better prevention tactics and more effective treatment choices. Keeping your exposure in check is a simple yet powerful way to protect your nails.
How Other Nail Issues Take a Different Path
Finger nail fungus typically owes its origin to environmental exposure and tiny, sometimes unnoticed injuries. However, other nail issues march to their own beat. Take nail psoriasis, for instance—it’s an immune-related reaction that creates thickened, pitted nails without the telltale fungal signs. On the other hand, a traumatic nail injury usually makes its presence known immediately after the incident, while fungal infections tend to creep up gradually. And then you have bacterial nail infections, which are marked by quick, jump-started inflammation and pain, making them quite distinct from the slow-burn nature of fungal issues.
These different developmental paths mean that when it comes to nail care, one size definitely doesn’t fit all. Understanding that not every discolored or misshapen nail is the same gives you a clearer roadmap on when and how to seek treatment. Recognizing whether repetitive stress, immune system quirks, or environmental exposures are at fault can make all the difference in getting the right help at the right time.
How Finger Nail Fungus is Diagnosed
The journey to a proper diagnosis for finger nail fungus starts with a thorough check-up by your healthcare provider. Your doctor will likely ask about your nail care habits, any past injuries, and possible exposures to fungal environments—all while giving your nail a close look at its texture, color, and overall condition. Often, the visual story told by your nail is enough to suggest a fungal infection, although additional tests might be needed to confirm the suspicion.
In many cases, your doctor could request laboratory tests like cultures and microscopic examinations to pinpoint the type of fungus involved. These tests play a crucial role in distinguishing it from other nail conditions such as psoriasis or bacterial infections, which require very different approaches. With both clinical observations and lab tests at hand, healthcare providers can confidently tailor the treatment, ensuring you receive an intervention plan that’s just right.
A Closer Look at What the Doctor Does
During a clinical evaluation, your healthcare provider takes notes on everything from the nail’s color and thickness to its texture. They’ll ask about your day-to-day habits, any previous nail mishaps, or past fungal issues you might have experienced. This hands-on approach gives a clear picture of whether the changes you’re seeing are due to finger nail fungus or something else entirely. Sometimes, specialized tools are even used to get a better look, ensuring nothing slips by unnoticed.
This blend of personal history and direct observation forms the backbone of an accurate diagnosis. By piecing together your experiences with what they see on your nail, your doctor can decide if further lab tests are needed—setting the stage for the right treatment.
Laboratory Tests and Microscopic Scrutiny
Often, lab tests are a key piece of the puzzle when it comes to confirming finger nail fungus. A small sample is taken from your affected nail and examined under a microscope to look for signs of fungal elements. Coupling this with cultures to identify the specific fungus helps decide on the best antifungal treatment. These precise methods are crucial in differentiating fungal infections from conditions like psoriasis or bacterial issues, which have their own set of diagnostic clues.
This microscopic peek into your nail provides that all-important extra layer of confirmation, ensuring that the treatment you receive is as targeted and effective as possible.